Introduction
Living with diabetes requires ongoing care, monitoring, and education—and nurses play a central role in ensuring patients maintain a healthy and balanced life. A nursing care plan (NCP) for diabetes is more than just a list of tasks; it’s a personalized roadmap that helps manage symptoms, prevent complications, and promote patient well-being. In this EssayAssits guide, we’ll walk you through everything you need to know about creating a professional nursing care plan for diabetes—complete with a free downloadable PDF template to get you started.
🩺 What Is a Nursing Care Plan for Diabetes?
A nursing care plan for diabetes mellitus is a structured document outlining a patient’s nursing diagnoses, goals, interventions, and outcomes related to managing diabetes. It provides a systematic approach for nurses to assess patient needs, track progress, and deliver evidence-based care.
This plan addresses the patient’s physical, emotional, and educational needs, helping them achieve better blood sugar control, avoid complications like neuropathy or retinopathy, and live a more independent life.
💡 Why Nursing Care Plans Matter in Diabetes Management
A nursing care plan (NCP) plays a vital role in ensuring effective and personalized diabetes management. Diabetes is a chronic condition that affects nearly every aspect of a patient’s life—diet, exercise, medication, emotional well-being, and long-term health outcomes. Without a structured care plan, it’s easy for important details to be overlooked, leading to inconsistent care or preventable complications.
Here’s why nursing care plans are essential in diabetes management:
- Ensure Consistency and Continuity of Care
A written care plan allows every nurse and healthcare provider involved to follow the same evidence-based strategy. Whether the patient is at home, in a hospital, or a long-term care facility, the plan ensures seamless communication and consistent care delivery. - Promote Early Detection of Complications
Diabetes increases the risk of serious complications such as neuropathy, retinopathy, and kidney disease. Through regular assessment and monitoring outlined in the care plan, nurses can spot early warning signs and take timely action to prevent worsening conditions. - Enhance Patient Education and Self-Management
Patient education is at the heart of every diabetes care plan. Nurses teach patients how to check blood sugar levels, recognize symptoms of hypo- or hyperglycemia, administer insulin, and make healthy lifestyle choices. This empowers patients to take charge of their own health and reduces dependency on hospital visits. - Facilitate Goal-Oriented and Personalized Care
Every diabetic patient has unique needs—some struggle with diet control, others with medication adherence. A nursing care plan allows nurses to set SMART goals (Specific, Measurable, Achievable, Realistic, and Time-bound) tailored to each patient’s situation. This individualized approach leads to better results and patient satisfaction. - Encourage Interdisciplinary Collaboration
Diabetes management often involves multiple healthcare professionals—physicians, dietitians, endocrinologists, and physical therapists. The care plan acts as a central communication tool, ensuring everyone is aligned and working toward the same objectives. - Improve Overall Health Outcomes
With structured interventions, clear goals, and continuous evaluation, nursing care plans lead to improved glycemic control, fewer hospital readmissions, and better quality of life for patients.
🧬 Common Nursing Diagnoses for Diabetes
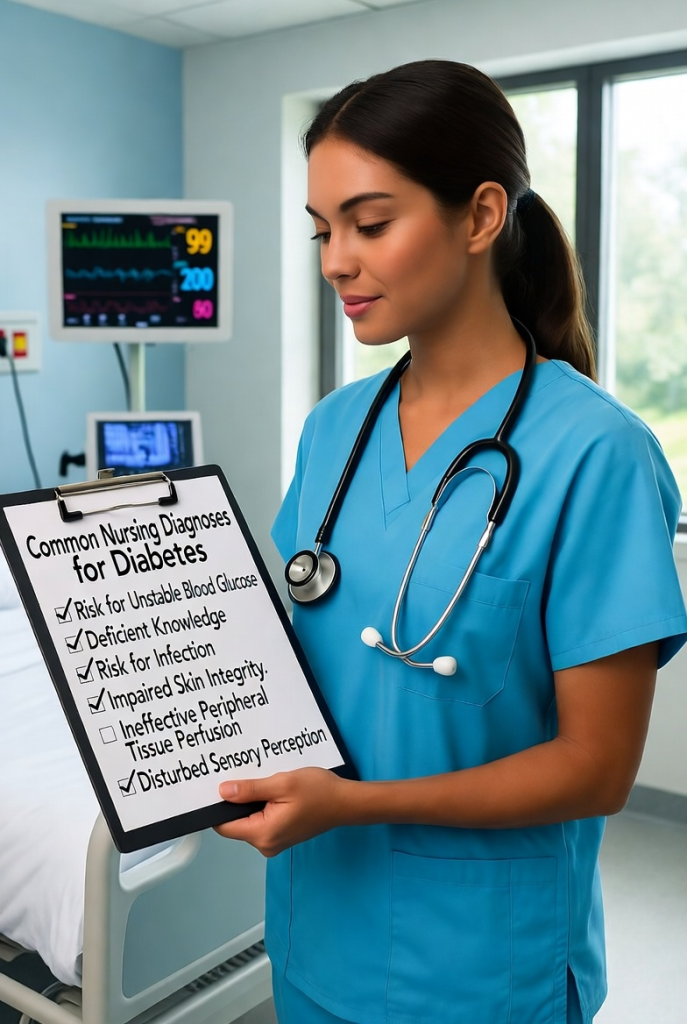
Creating a comprehensive diabetes nursing care plan begins with identifying accurate nursing diagnoses—the foundation for all interventions and outcomes. These diagnoses guide nurses in addressing both the physical and psychosocial aspects of the condition, helping patients achieve better blood sugar control and overall well-being.
Here are the most common nursing diagnoses used for patients with diabetes mellitus:
1. Ineffective Health Management
Related to: Insufficient knowledge of diabetes control, complex medication regimen, or lack of motivation.
As evidenced by: Inconsistent glucose monitoring, poor adherence to diet, or frequent episodes of hyper/hypoglycemia.
Goal: Patient will demonstrate effective self-management behaviors, including blood sugar monitoring and medication adherence.
2. Risk for Unstable Blood Glucose Levels
Related to: Inconsistent dietary intake, physical activity variations, illness, or medication side effects.
Goal: Maintain blood glucose levels within the target range (e.g., fasting 80–130 mg/dL).
Interventions:
- Monitor blood sugar levels regularly.
- Educate on balanced meal planning.
- Reinforce the importance of medication timing and dosage.
3. Risk for Infection
Related to: Decreased circulation, delayed wound healing, or neuropathy.
As evidenced by: Open wounds, poor skin turgor, or elevated blood glucose levels.
Goal: Patient will remain free from signs of infection.
Interventions:
- Inspect feet and skin daily.
- Educate on proper wound and foot care.
- Encourage good personal hygiene and blood sugar control.
4. Deficient Knowledge (Disease Process and Management)
Related to: New diagnosis, lack of understanding, or misinformation.
As evidenced by: Frequent questions about medication, diet, or blood sugar monitoring.
Goal: Patient will verbalize understanding of diabetes management and demonstrate correct self-care techniques.
Interventions:
- Provide educational materials and demonstrations.
- Assess learning readiness and comprehension.
- Reinforce positive lifestyle changes.
5. Imbalanced Nutrition: More Than Body Requirements
Related to: Excessive food intake, sedentary lifestyle, or poor dietary habits.
As evidenced by: Weight gain, elevated blood glucose, or BMI > 25.
Goal: Achieve and maintain a healthy weight through balanced nutrition and exercise.
Interventions:
- Collaborate with a dietitian to create an individualized meal plan.
- Encourage regular physical activity.
- Teach portion control and label reading.
6. Risk for Injury
Related to: Decreased sensation (neuropathy), poor vision (retinopathy), or hypoglycemia episodes.
Goal: Prevent injuries and maintain a safe environment.
Interventions:
- Assess sensory deficits and provide safety education.
- Encourage the use of protective footwear.
- Teach family members how to recognize and manage hypoglycemia.
7. Fatigue
Related to: Inadequate glucose utilization or altered metabolic state.
As evidenced by: Reports of exhaustion, low energy, or difficulty performing activities.
Goal: Patient will verbalize improved energy levels.
Interventions:
- Encourage balanced rest and activity periods.
- Monitor blood sugar and adjust interventions accordingly.
- Promote adherence to prescribed treatment.
8. Disturbed Sensory Perception (Tactile/Visual)
Related to: Diabetic neuropathy or retinopathy.
As evidenced by: Tingling, numbness, or vision changes.
Goal: Minimize sensory impairment and prevent injury.
Interventions:
- Schedule regular ophthalmologic and neurological assessments.
- Educate on foot protection and proper footwear.
- Monitor for progression of sensory changes.
🩺 EssayAssits Insight
Nursing diagnoses form the core of individualized diabetes care. Each diagnosis should be patient-specific, measurable, and linked to actionable interventions. By combining clinical judgment with patient education, nurses can transform these diagnoses into meaningful improvements in health outcomes.
Would you like me to include a formatted nursing diagnosis table (with columns for diagnosis, goal, and intervention) to make it look more professional for your blog or PDF template?
Here’s a comprehensive and practical breakdown of Nursing Interventions for Diabetes, written in the EssayAssits way — clear, professional, and tailored for nursing students and practitioners.
💉 Nursing Interventions for Diabetes
Effective nursing interventions for diabetes focus on maintaining stable blood glucose levels, promoting self-management, and preventing both short- and long-term complications. Each intervention should be evidence-based, patient-centered, and adaptable to individual needs.
1. Blood Glucose Monitoring
Intervention:
- Monitor blood glucose levels regularly (as prescribed or every 4–6 hours for inpatients).
- Record and report abnormal readings promptly.
Rationale:
Continuous monitoring helps detect trends, prevent hypoglycemia or hyperglycemia, and guide medication adjustments.
2. Administer Medications as Prescribed
Intervention:
- Administer insulin or oral hypoglycemic agents accurately and on time.
- Monitor for adverse effects such as hypoglycemia, dizziness, or allergic reactions.
Rationale:
Proper medication adherence ensures glucose control and prevents acute metabolic complications.
3. Promote Nutritional Management
Intervention:
- Collaborate with a dietitian to develop an individualized meal plan.
- Educate the patient about carbohydrate counting, portion control, and label reading.
- Encourage consistent meal timing to align with insulin schedules.
Rationale:
Balanced nutrition supports stable glucose levels and prevents energy fluctuations.
4. Encourage Regular Physical Activity
Intervention:
- Recommend moderate exercise (e.g., walking 30 minutes daily, 5 times per week).
- Monitor blood glucose before and after exercise to prevent hypoglycemia.
- Encourage hydration and rest as needed.
Rationale:
Exercise enhances insulin sensitivity, promotes weight management, and improves circulation.
5. Provide Diabetes Education
Intervention:
- Teach proper insulin injection techniques and self-monitoring of blood glucose (SMBG).
- Explain signs and management of hypo- and hyperglycemia.
- Educate on long-term complications (neuropathy, retinopathy, nephropathy) and prevention strategies.
Rationale:
Education empowers patients to take responsibility for their health and reduces hospital readmissions.
6. Prevent Skin Breakdown and Foot Complications
Intervention:
- Inspect the patient’s skin, especially feet, daily for cuts, blisters, or infections.
- Teach foot care practices: daily washing, drying, and wearing well-fitting shoes.
- Avoid applying heat or harsh chemicals to feet.
Rationale:
Poor circulation and neuropathy in diabetics increase the risk of ulcers and amputations.
7. Encourage Adequate Hydration
Intervention:
- Encourage intake of sugar-free fluids, unless contraindicated.
- Monitor for signs of dehydration such as dry mouth and poor skin turgor.
Rationale:
Adequate hydration helps flush excess glucose through urine and maintains electrolyte balance.
8. Monitor for Signs of Complications
Intervention:
- Assess for symptoms of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS).
- Check for neuropathy, visual changes, and delayed wound healing.
Rationale:
Early recognition of complications allows for immediate medical intervention.
9. Provide Emotional and Psychosocial Support
Intervention:
- Assess the patient’s coping mechanisms and emotional state.
- Offer counseling or refer to support groups if needed.
- Encourage family participation in care planning.
Rationale:
Emotional support enhances motivation, compliance, and overall quality of life.
10. Reinforce Adherence to the Care Plan
Intervention:
- Review goals with the patient regularly.
- Use motivational interviewing to address barriers to self-care.
- Praise progress and provide feedback.
Rationale:
Consistent reinforcement improves patient engagement and long-term outcomes.
🧠 EssayAssits Tip
When documenting interventions:
- Always link them to the specific nursing diagnosis and goal.
- Include frequency, duration, and evaluation criteria.
- Use clear, action-oriented language (e.g., “Monitor,” “Teach,” “Encourage,” “Assess”).
🩺 Key Components of a Diabetes Nursing Care Plan
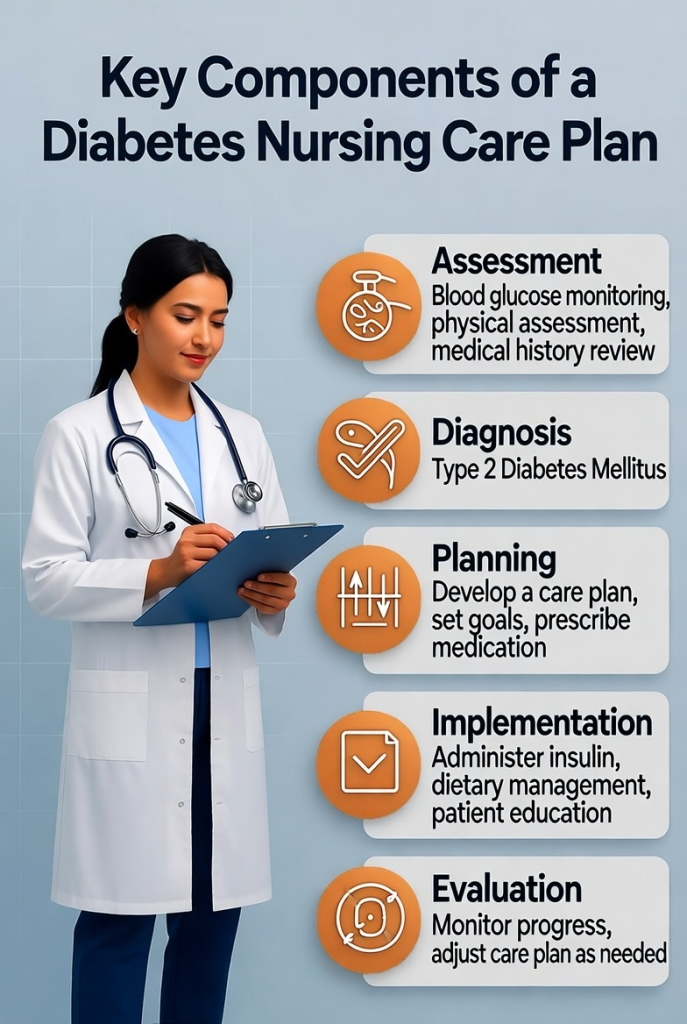
A Diabetes Nursing Care Plan serves as a roadmap for delivering personalized, evidence-based care to patients managing diabetes mellitus. It helps nurses address physical, psychological, and educational needs to promote long-term wellness and prevent complications. Below are the core components every effective plan should include:
1. Assessment
The first step involves gathering relevant patient data to form a baseline for care.
Key aspects include:
- Health history: duration of diabetes, medication use, family history, comorbidities.
- Physical assessment: weight, BMI, skin condition (especially feet), hydration status.
- Laboratory results: blood glucose levels, HbA1c, lipid profile, renal function tests.
- Lifestyle factors: diet, exercise routine, stress levels, smoking, alcohol use.
- Psychosocial assessment: emotional state, coping mechanisms, support system.
2. Nursing Diagnoses
Based on the assessment, nurses identify current and potential health issues.
Common nursing diagnoses include:
- Imbalanced nutrition: more or less than body requirements
- Risk for unstable blood glucose levels
- Deficient knowledge related to disease management
- Risk for impaired skin integrity
- Ineffective health management
3. Planning (Goals and Outcomes)
This step sets measurable, realistic, and time-bound goals.
Examples of goals:
- Patient will maintain blood glucose within the target range (e.g., 80–130 mg/dL fasting).
- Patient will verbalize understanding of self-care techniques by discharge.
- Patient will demonstrate proper insulin administration techniques.
4. Nursing Interventions
These are specific nursing actions aimed at achieving the goals.
Examples:
- Monitor blood glucose and vital signs regularly.
- Educate the patient on insulin use, dietary choices, and exercise importance.
- Encourage adherence to medication and blood glucose monitoring schedules.
- Assess for signs of hypo- or hyperglycemia.
- Collaborate with dietitians, endocrinologists, and educators for holistic care.
5. Rationale
Each intervention should be supported by a scientific explanation.
For example:
“Monitoring blood glucose helps identify trends and prevent acute complications like hypoglycemia or ketoacidosis.”
6. Evaluation
This step measures the effectiveness of interventions and patient progress.
Evaluation questions:
- Is the patient’s blood glucose within the target range?
- Has the patient demonstrated correct self-monitoring and insulin techniques?
- Are lifestyle modifications being followed consistently?
If goals are unmet, revise the plan accordingly.
7. Documentation
Accurate, timely, and detailed documentation ensures continuity of care.
Record all findings, nursing actions, patient responses, and changes in condition.
🧠 EssayAssits Tip
When writing or presenting your nursing care plan, focus on clarity, patient-centered care, and evidence-based rationale. Use simple, concise language and avoid medical jargon when explaining concepts to patients.
Would you like me to include a sample Diabetes Nursing Care Plan table (Assessment → Diagnosis → Goals → Interventions → Evaluation) in a downloadable PDF format?
🩹 Sample Nursing Care Plan for Diabetes
| Nursing Diagnosis | Goals/Outcomes | Nursing Interventions | Rationale | Evaluation |
| Risk for Unstable Blood Glucose Levels | Maintain fasting blood glucose between 80–130 mg/dL | – Monitor glucose levels regularly- Administer insulin as prescribed- Educate on diet and activity | Monitoring and education improve glycemic control | Blood glucose maintained within target range |
| Deficient Knowledge related to disease process | Patient verbalizes understanding of diabetes management | – Provide teaching on signs of hypo/hyperglycemia- Review medication adherence- Offer printed education materials | Knowledge improves self-care and reduces complications | Patient demonstrates understanding through self-monitoring |
📘 Download Your Free Nursing Care Plan PDF Template
To make your work easier, EssayAssits has created a free downloadable and editable PDF template you can use for your next care plan. It includes all essential sections—assessment, diagnosis, interventions, and evaluation—formatted for quick charting and professional presentation.
👉 [Download the Free Diabetes Nursing Care Plan PDF Template] (link placeholder)
🧠 Tips for Writing an Effective Nursing Care Plan (The EssayAssits Way)
- Personalize every plan: Adapt goals and interventions to each patient’s unique condition and lifestyle.
- Use evidence-based interventions: Rely on the latest clinical guidelines from ADA or WHO.
- Focus on patient education: Empower patients to take control of their health.
- Document clearly: Use concise and measurable language for better communication among care teams.
- Review and update: Regularly adjust the plan based on patient progress.
❓ FAQs: Diabetes Nursing Care Plan

1. What is a Diabetes Nursing Care Plan?
A Diabetes Nursing Care Plan is a structured guide that helps nurses manage and monitor the care of patients with diabetes mellitus. It includes assessment, diagnosis, interventions, goals, and evaluation steps designed to promote blood glucose control and prevent complications.
2. Why is a Nursing Care Plan Important for Diabetes?
It ensures individualized care, promotes consistency among healthcare providers, and enhances patient education and self-management. The plan also helps prevent serious complications such as neuropathy, retinopathy, and cardiovascular diseases.
3. What are the Main Goals of Diabetes Care?
- Maintain normal or near-normal blood glucose levels.
- Prevent acute complications like hypoglycemia and hyperglycemia.
- Promote healthy lifestyle changes such as diet control and regular exercise.
- Improve quality of life and patient independence.
4. What Nursing Interventions Are Most Effective for Diabetes Management?
Some key interventions include:
- Monitoring blood glucose regularly.
- Educating patients about insulin use and diet.
- Encouraging adherence to treatment and exercise plans.
- Assessing for early signs of infection or neuropathy.
- Providing emotional and psychological support.
5. How Often Should a Nursing Care Plan Be Updated?
A care plan should be reviewed and updated regularly, especially when:
- The patient’s condition changes.
- New laboratory results become available.
- The patient starts a new medication or therapy.
6. Can Patients Participate in Their Own Care Plan?
Absolutely! Involving patients enhances adherence and accountability. Nurses should encourage self-monitoring, goal setting, and education to empower patients to take control of their health.
7. What’s the Difference Between Type 1 and Type 2 Diabetes in Nursing Care Plans?
- Type 1 Diabetes: Focuses on insulin administration, glucose monitoring, and preventing hypoglycemia.
- Type 2 Diabetes: Emphasizes lifestyle modification, oral medication adherence, and weight management.
8. How Can Nurses Educate Patients About Diabetes?
By teaching practical skills such as:
- How to use a glucometer.
- Reading food labels and planning balanced meals.
- Recognizing signs of hypo/hyperglycemia.
- Stress management and foot care techniques.
9. What Challenges Do Nurses Face in Diabetes Management?
Common challenges include poor patient adherence, limited resources, language barriers, and managing comorbid conditions. Consistent education and motivational interviewing can help overcome these issues.
10. Where Can I Find a Sample Diabetes Nursing Care Plan Template?
You can download a free, editable Diabetes Nursing Care Plan PDF Template from EssayAssits, designed for both nursing students and professionals who want to organize their patient care efficiently.
Would you like me to create that free downloadable Diabetes Nursing Care Plan PDF template (including sample goals, diagnoses, and interventions)?
🩷 Final Thoughts
Creating a nursing care plan for diabetes isn’t just a nursing requirement—it’s a powerful tool for patient empowerment and better health outcomes. By following the EssayAssits approach—clear, structured, and patient-centered—you can deliver professional, compassionate, and effective diabetes care every time.
With your free PDF template, you’ll be equipped to streamline documentation and focus more on what truly matters: helping patients live healthier lives.
Creating an effective Diabetes Nursing Care Plan is more than just fulfilling a nursing requirement — it’s about empowering patients to live healthier, more independent lives. By combining clinical knowledge, patient-centered care, and continuous evaluation, nurses play a critical role in managing diabetes and preventing life-threatening complications.
A well-structured care plan helps identify patient needs early, set realistic goals, and apply evidence-based interventions. It also fosters collaboration between patients, nurses, and the healthcare team, ensuring long-term success in managing both Type 1 and Type 2 diabetes.
At EssayAssits, we believe that nursing care plans should be clear, comprehensive, and actionable. Whether you’re a nursing student or a practicing professional, using a structured approach makes it easier to deliver quality care and achieve positive outcomes.
💡 Final EssayAssits Tip: Always update your care plan as the patient’s condition evolves — nursing care is a continuous process of assessment, action, and improvement.
